If you reside in the rural U.S., you are well aware that access to timely medical care is not always convenient. Driving long distances to the nearest hospital, a lack of specialists, and few healthcare resources make even something as basic as an annual check-up a challenge.
That’s where Remote Patient Monitoring (RPM) is beginning to make a significant impact. By monitoring your health at home using connected devices, RPM enables physicians to monitor your condition without you having to go into town. For rural populations, this technology is not just convenient – it’s revolutionizing the delivery of healthcare.
The Everyday Challenges of Rural Healthcare
The rural clinics and hospitals are challenged in certain ways that city facilities never see. Most communities don’t have enough doctors and specialists to go around, leading to wait times longer than an hour and crowded clinics. Geography can be a barrier too – for some patients, a 50- or 100-mile drive for an appointment is entirely routine.
On top of that, smaller health centers tend to have tight budgets, restricting their capacity to purchase the newest and best medical equipment or add more professionals. All these put together create a system where individuals tend to postpone care until an issue is serious, resulting in worse results and increased expenditures.
What is Remote Patient Monitoring?
Remote Patient Monitoring uses digital technology to capture your medical data, like blood pressure, glucose levels, or oxygen saturation, and transmit it securely to your healthcare provider in real time.
It’s like having a personal check-up station right in your home. Your doctor can review the data regularly, spot any early warning signs, and reach out before a minor issue turns into a medical emergency. For people managing chronic conditions, this kind of early detection can be life-changing.
Why RPM Works So Well in Rural Areas?
For rural communities, RPM removes one of the biggest barriers to healthcare: distance. Rather than spending hours commuting to a clinic for basic monitoring, patients can report their health information from home. Not only is it more convenient, but patients are also more likely to engage in their healthcare.
RPM adoption among hospitals surged from 42 percent in 2018 to 58 percent in 2022, showing how rapidly this technology is becoming integrated into modern care.
Ongoing monitoring allows issues to be detected and treated sooner, sometimes before symptoms ever occur. And by avoiding unnecessary emergency room visits or hospitalization, RPM can save considerable expenses for both patients and the healthcare system.
New Ways Rural Providers Are Leveraging RPM
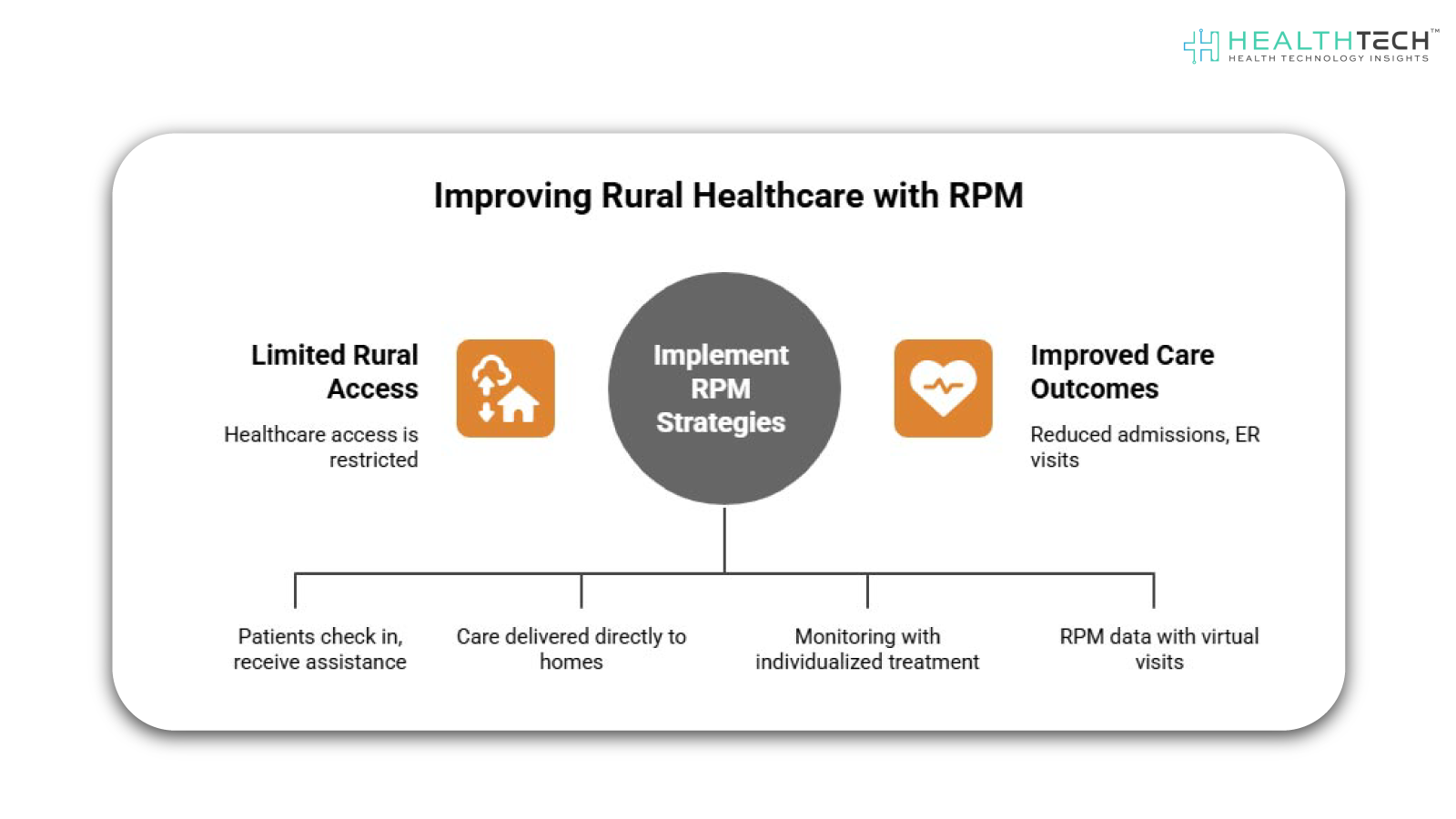
Rural providers are getting creative about how to incorporate RPM into their models of care. Some have established community health hubs where patients come in to check in, see monitoring equipment, and receive assistance with uploading their information. Others have mobile health units that are equipped with RPM technology and travel out to rural communities, bringing care directly to those who need it most. Implementing RPM has led to a 32% reduction in hospital admissions and a 14% drop in emergency department visits, dramatically improving care outcomes in rural populations.
Numerous hospitals have initiated standalone programs for chronic conditions such as diabetes, heart disease, or hypertension, coupling ongoing monitoring with individualized treatment regimens. Telehealth alliances are also on the rise, enabling providers to blend RPM data with virtual visits so patients can consult specialists in their homes. These strategies are making RPM accessible and convenient for rural dwellers.
The Speed Bumps RPM Still Faces
Although the potential of RPM is vast, there are still obstacles to be overcome in order for it to be widely used in rural settings. Perhaps the greatest obstacle is internet connectivity; without stable broadband, real-time transmission of health information can prove problematic. A second factor is digital literacy, where patients and providers must be trained to effectively utilize the devices and platforms.
Insurance coverage for RPM also differs from state to state, and in some instances, reimbursement rates don’t pay for the entire cost of implementation. And of course, data privacy and security are still top-of-mind issues, demanding stringent protections to ensure the confidentiality of sensitive health information. Defining the resolutions for these challenges will necessitate close cooperation among healthcare providers, technology firms, and policymakers, but solutions are already underway.
How Remote Patient Monitoring Empowers Patients?
The future of Remote Patient Monitoring in rural medicine is bright. As broadband penetration increases, devices become easier to use, and policy backing increases, RPM might well become a routine part of rural American care. Though it will never displace in-person visits entirely, it will make healthcare much more proactive, accessible, and patient-focused. To rural citizens, that might translate to fewer doctor visits, earlier diagnosis of ailments, and greater mastery over their health.
FAQs
1. What is Remote Patient Monitoring (RPM)?
RPM refers to the utilization of electronic devices to capture patients’ health information, e.g., blood pressure, heart rate, or glucose levels, and forward it to healthcare professionals for remote monitoring and prompt interventions.
2. How does RPM help rural communities?
RPM enhances care access, lowers the requirement for out-of-territory travel, facilitates early detection of medical issues, boosts patient involvement, and can reduce healthcare expenses through hospital readmission prevention.
3. What kind of conditions can RPM track?
RPM is mostly applied to chronic conditions such as diabetes, high blood pressure, heart disease, and respiratory diseases. It can also aid post-surgical rehabilitation and care for the elderly.
4. What kind of technology does RPM need?
Patients most commonly use linked devices like blood pressure monitors, glucometers, pulse oximeters, or wearable monitors. An internet connection or cellular network is required to send data to providers.
5. Are there challenges to implementing RPM in rural settings?
Yes, among them are limited access to the internet, lack of digital literacy, variable insurance reimbursement, and data privacy and security concerns.Dive deeper into the future of healthcare – Keep reading on Health Technology Insights.To participate in our interviews, please write to our HealthTech Media Room at sudipto@intentamplify.com