When was the last time your healthcare system made money by staying connected, without anyone walking into a building? It’s the reality of Telehealth 3.0, and it’s already happening in health systems that have decided to stop treating telehealth like a backup plan and start treating it like a core part of how care is delivered.
Telehealth is no longer just about video visits or post-pandemic convenience. It’s about creating a continuous care experience that improves outcomes, lightens the load for clinical teams, and delivers serious ROI.
What Is Telehealth 3.0?
Think of it this way:
- Telehealth 1.0 got us online. It made care accessible when the world shut down.
- Telehealth 2.0 made it easier and more integrated. Great for follow-ups and reducing wait times.
- Telehealth 3.0? It’s a 24/7 digital care environment. One that watches over patients long after the visit ends.
It uses:
- Remote monitoring devices that catch warning signs in real time.
- AI that knows when to escalate and when to nudge.
- Virtual nurses who can jump in and handle key touchpoints.
- Platforms that personalize outreach and automate what doesn’t need to be manual.
It’s continuous, connected, and subtly changing the way health systems function.l
Where is the ROI, then?
With Telehealth 3.0, we’re seeing actual, trackable return on investment. Let’s walk through how.
1. Fewer Readmissions, Happier Finance Teams
We all know how much avoidable readmissions cost. They’re bad for patients, bad for ratings, and really bad for budgets.
But imagine this: A heart failure patient’s weight creeps up overnight. A connected scale sends an alert. A virtual nurse checks in, adjusts meds, and avoids a trip to the ER.
That’s exactly what’s happening in real life. Some hospitals have seen more than 30% drops in readmissions. That translates into millions in saved costs and better patient outcomes.
2. Smarter Staffing
Nurses are exhausted. Clinicians are overwhelmed. Hiring more bodies just isn’t scalable anymore. That’s where virtual nursing and automation step in, not to replace humans, but to support them.
Imagine a nurse handling patient education from home. Or AI listening in and auto-filling documentation, so your doctor isn’t up till midnight with her laptop.
Systems using virtual care models are cutting overtime, burnout, and reliance on expensive staffing agencies. And they’re seeing real relief for people and budgets.
3. Patients Stick Around When They Feel Seen
Here’s a truth that’s easy to overlook: Patients want to be remembered.
They want a system that checks in between visits. That reminds them to refill a prescription. That says, “Hey, how are you feeling today?”
Telehealth 3.0 makes that possible with the help of smart reminders, check-ins, and connected dashboards. And when patients feel supported, they’re more likely to stay with your system.
That translates to higher retention, more referrals, and stronger lifetime value.
4. Tech That Fits Into Your System
Old-school telehealth platforms were rigid and expensive. But today’s solutions? They are modular, cloud-native, and designed to change to meet your needs. Start small, scale up, connect to your current systems, and get rid of the cumbersome infrastructure.
Faster time to value, reduced TCO (total cost of ownership), and fewer IT issues are the results.
5. It Moves the Needle on Value-Based Care
Payers are watching. So are quality scores. When you’re operating in a value-based world, every avoided hospitalization, every better-controlled A1C, every completed follow-up matters.
Telehealth 3.0 helps you deliver those wins. And that leads to bonuses, better contracts, and stronger negotiating power.
This is how some systems are already outperforming benchmarks, and getting paid for it.
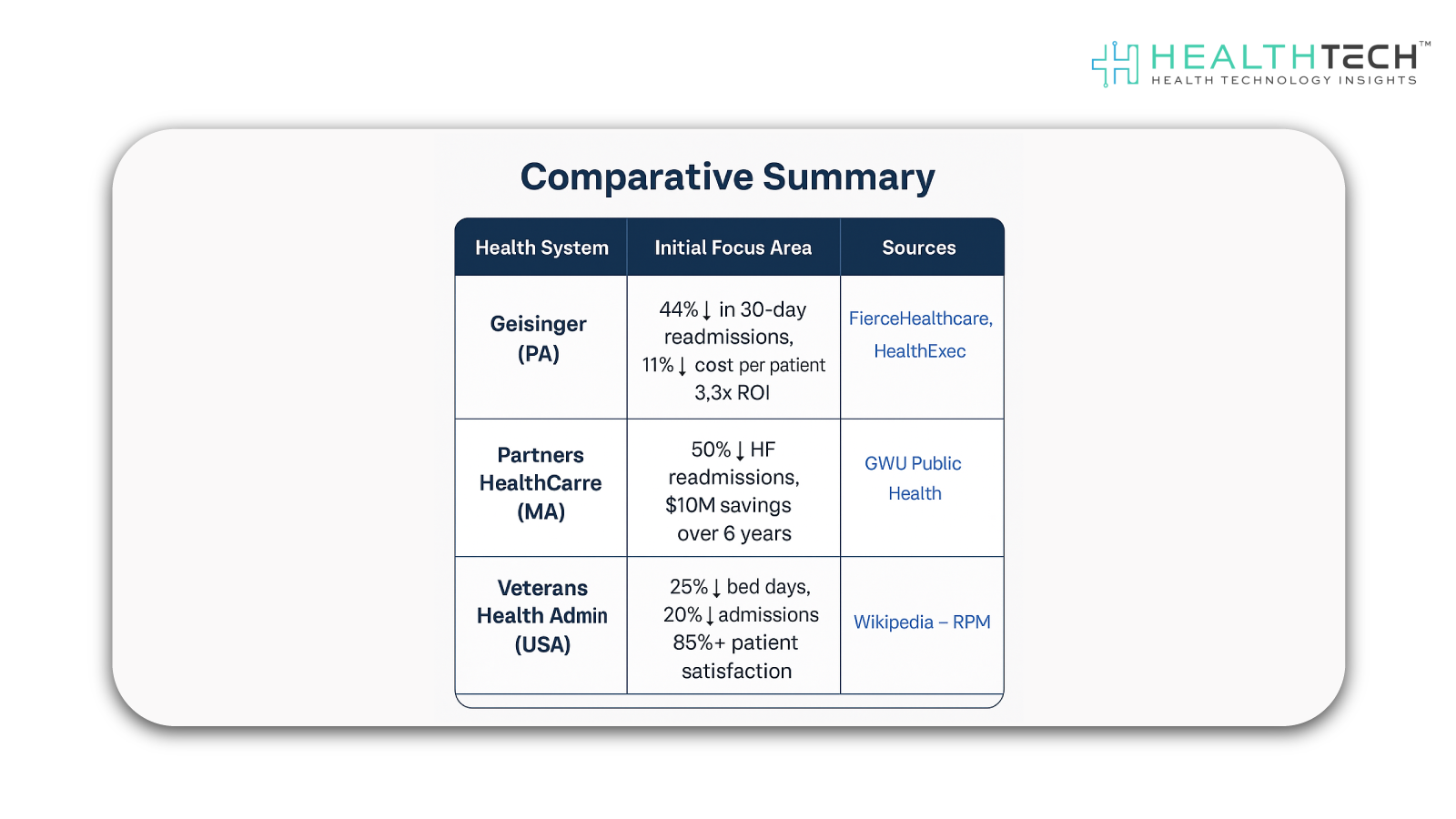
Geisinger Health System: Heart Failure Telemonitoring Program
Using automated phone-based IVR (Interactive Voice Response), nurse follow-ups, and RPM technology, Geisinger, a significant U.S. health institution with its headquarters located in Pennsylvania, started a telemonitoring program tailored for patients with heart failure. This was a planned attempt to cut down on avoidable readmissions and the expenses associated with providing care to high-risk groups.
Important Results:
- 30-day readmissions among enrolled patients were reduced by 44%.
- 11% less money is spent on each patient than on standard care.
- Reduced preventable hospitalizations and staff resource use resulted in a 3.3x net return on investment.
- Enhanced patient involvement through care coordination and daily check-ins.
What Makes This Work?
Here’s what separates high-ROI systems from the rest:
Data that connects
If your tools don’t talk to each other, nothing works. The best platforms plug into your EHR, your patient portals, and your monitoring devices seamlessly.
Workflows built for real people
The tech should adapt to your teams, not the other way around. It should save time, not add complexity.
Leadership that gets it
You need your CFO, CMO, CIO, and clinical leaders aligned. This isn’t “just a digital tool.” It’s infrastructure.
A focus on outcomes, not vanity metrics
Don’t chase virtual visit volume. Track the stuff that matters: fewer ED visits, better quality scores, lower total cost of care.
Extending Care Beyond Limits with Telehealth 3.0
Telehealth 3.0 isn’t about replacing care, it’s about extending it. It helps you show up for patients when it matters most, without adding more bricks and mortar or burning out your teams.
It’s smart, scalable, and sustainable. The organizations that lean into it now are not just improving care. They’re building the financial and operational resilience healthcare needs next.
FAQs
1. How is Telehealth 3.0 different from the earlier versions of virtual care?
Telehealth 1.0 was all about basic video visits, and 2.0 expanded to include some digital tools. But Telehealth 3.0 is a whole new mindset; it’s not just about appointments, it’s about continuous, connected care.
2. What kind of ROI can health systems expect from investing in Telehealth 3.0?
The ROI is both clinical and financial. Health systems are seeing fewer readmissions, better chronic condition management, reduced ED visits, and stronger patient engagement. Financially, this translates to lower operating costs, higher reimbursements in value-based care models, and improved resource utilization.
3. Do patients want more virtual care, or is it just a system-driven trend?
Patients are driving the demand for smarter, more convenient care. Many now expect their healthcare to be as seamless as their favorite apps. What they want isn’t just virtual visits, it’s proactive, always-on support, especially for managing chronic conditions.
4. What are the biggest challenges in adopting Telehealth 3.0 across a health system?
Change management is a big one. It requires aligning clinical workflows, training staff, updating infrastructure, and ensuring interoperability across platforms. Reimbursement models can also lag behind the tech.
5. How does Telehealth 3.0 impact clinicians and care teams?
Surprisingly positively. When done right, it reduces the burden of redundant tasks, supports smarter triaging, and gives clinicians better visibility into patients’ day-to-day health. This leads to more meaningful interactions and less burnout.
Dive deeper into the future of healthcare.
Keep reading on Health Technology Insights.
To participate in our interviews, please write to our HealthTech Media Room at sudipto@intentamplify.com