This piece captures expert interpretation of where the recent FDA green light for Neuralink’s Blindsight implant intersects with health-tech strategy, neuroprosthetics development, and the practical challenges leaders face in adopting disruptive biomedical technologies.
In the raw calculus of medtech breakthroughs and investment narratives, a line often gets drawn between promise and proof. For health-tech leaders and clinical decision-makers today, the U.S. (FDA) Food and Drug Administration’s recent breakthrough designation for Neuralink’s Blindsight implant feels like a moment frozen between those two.
It signals that a device once confined to speculative science fiction now stands within a recognized pathway toward clinical evaluation and, potentially, widespread use. That carries implications that ripple beyond Neuralink and its high-profile founder.
How Blindsight Intends to Bypass the Eye Entirely
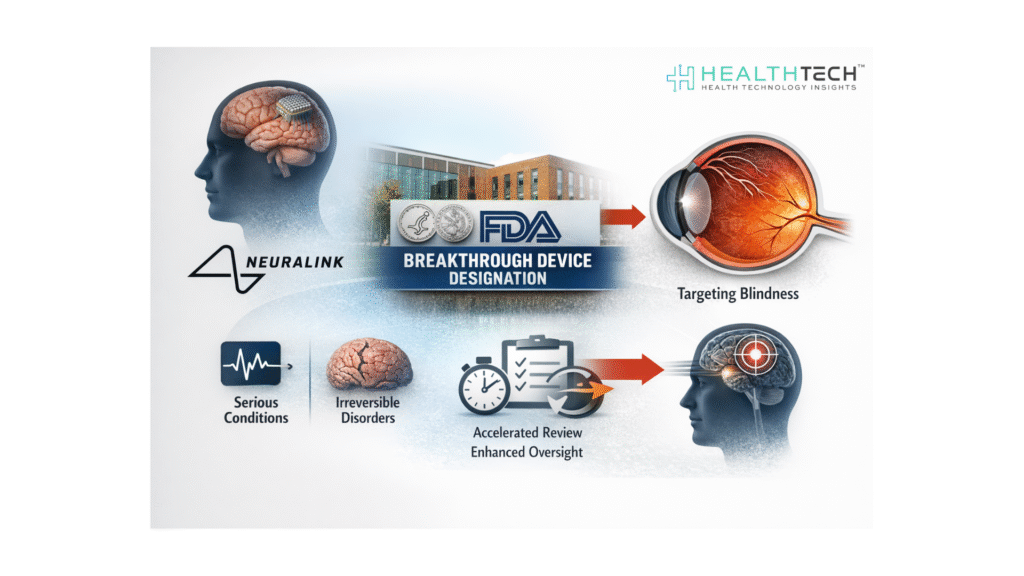
The core proposition of Blindsight is straightforward: directly stimulate the brain’s visual cortex with an implanted microelectrode array to restore perception in individuals whose optic nerves are non-functional. That means bypassing decades of entrenched assumptions about irreversible blindness due to nerve damage.

Source: Metaverse Planet
What makes this more than theoretical is the FDA’s breakthrough device designation, intended to expedite evaluation of technologies “that may provide more effective treatment” for debilitating conditions. That status doesn’t equate to market approval, but it does compress timelines and enhances regulatory feedback loops for developers.
“Blindsight will enable those who have total loss of vision… to be able to see again,” tweeted Elon Musk.
Critically, this regulatory cue came on the basis of preliminary evidence and preclinical data, not definitive human results. Musk has publicly suggested the device may function first as low-resolution vision – “Atari graphics,” in his words – with the possibility for enhancements over time, including perception beyond the normal human visual spectrum.
That aspiration captures imagination, but it also shifts the conversation from feasibility to fidelity of perception. Early trials will likely quantify what signals mean in practice – blurred movement versus distinct shapes, for example – and whether users can integrate these visual data into meaningful interaction with their environment.
Where Clinical Need Outpaces Clinical Data
Neuralink has occupied an unusual amount of mindshare for a company still early in clinical validation. That attention sharpened this week when the company disclosed it had received a breakthrough device designation from the U.S. FDA for its Blindsight implant.
The designation is reserved for medical devices intended to treat or diagnose life-threatening or irreversibly debilitating conditions, and it is designed to accelerate regulatory review through closer FDA engagement. It is a procedural signal, not a clinical endorsement. But it does place Blindsight on a faster, more closely supervised development track than conventional neuroprosthetic programs.
Blindsight raises familiar tensions: innovation versus evidence, hope versus expectation, and regulatory progress versus clinical readiness. In treating irreversible blindness, there are few real alternatives today. Gene therapies targeting specific genetic forms of retinitis pigmentosa and optogenetics are advancing, but none yet offer a general solution for damage at the optic nerve level. This is precisely the clinical gap that Blindsight aims to fill.
The Evidence Gap Between Neural Signals and Sight
To date, the most solid reported evidence of an implanted Brain-Computer Interface (BCI) device from Neuralink has involved enabling individuals with quadriplegia to control digital interfaces via neural signals.
Those cases offer proof of concept for safety and signal decoding, but they are not vision restoration outcomes. Without peer-reviewed human data showing reliable transmission of spatially coherent visual information, any projection of efficacy rests on extrapolation from animal models and early engineering benchmarks.
This isn’t to dismiss Blindsight’s promise. There is strong mechanistic logic: if a microelectrode array can reliably stimulate visual cortex neurons in patterns the brain interprets as structured visual input, then perception could emerge from stimulation sans retina. This is similar in concept to cochlear implants for hearing loss, where electrical stimulation of auditory nerves can restore functional hearing.
But cochlear implants took decades of design iteration and patient training to become the standard of care. Neuralink’s version compresses these expectations into years rather than decades, and that compression invites risk.
Health Tech Insights Perspective
From a Health Tech Insights lens, three strategic issues deserve scrutiny:
1. Clinical Evidence and Endpoints
Regulatory designation is not clinical validation. As Blindsight enters early human trials, leaders must differentiate between novel signal detection and clinically meaningful vision restoration.
Functional endpoints – such as navigation ability, object recognition, or quality-of-life metrics – must be defined by clinicians, not just engineers.
2. Safety Profile and Long-term Integration
Neural implants carry unique risk vectors- infection, tissue reaction, signal degradation over time, and the challenge of explantation. Longitudinal data will matter more than short-term performance metrics.
The field has grappled with these in spinal cord stimulators and deep brain stimulation; there will be parallels here, but also unprecedented questions about visual cortex engagement.
3. Ethical and Equitable Access Considerations
Blindsight, like many frontier neurotechnologies, carries potential for deep impact but also for stark disparities, such as:
Who gets prioritized for early access? How do payers evaluate value in the absence of long-term outcomes?
And how does deployment align with broader health equity goals?
Regulators have labeled the device promising enough to expedite, but that label doesn’t answer access and reimbursement questions that will influence adoption and investment.
Measured Disruption in a Crowded Neurotech Landscape
There is also a broader context: the neurotech field is proliferating. Competing approaches, such as non-invasive neurostimulation, retinal prosthetics, and gene therapies targeting photoreceptor degeneration, remain active. Some offer incremental benefits with lower procedural risk.
Blindsight’s differentiator – direct cortical engagement – is technically impressive, but it also entails the highest complexity. The choice for health systems will not be binary adoption or rejection, but calibrated evaluation against performance, risk, and cost.
For biotech investors and strategic partners, the Blindsight milestone will likely reshape risk-adjusted return models for neuroprosthetics. A breakthrough designation, even without approval, signals regulatory openness to bold devices.
That could accelerate capital flow into adjacent technologies focusing on neurorehabilitation, sensory substitution, and cognitive augmentation. The question then becomes not whether this wave of innovation will come, but which engines of that wave generate replicable, scalable clinical value. Evidence and reproducibility will be the currency.
Musk’s personal brand looms large over this narrative. There is a risk of conflating charismatic prediction with clinical fact. Industry veterans know that transformative health technologies almost always look unimpressive at first. Magnetic resonance imaging (MRI) was computationally primitive at birth. Cochlear implants were rudimentary.
What matters is the trajectory from theoretical viability to consistent, reproducible patient outcomes. That typically involves transparent reporting, peer-reviewed trials, and iterative refinement – disciplines that sit uncomfortably alongside hype and ambition.
Reading Past the Breakthrough Label
Where does this leave health-tech leaders today? If you are allocating research investment, the Blindsight moment suggests that neuroprosthetics is maturing from laboratory curiosity to a regulated clinical domain.
That could recalibrate funding priorities toward interfaces and signal interpretation technologies rather than purely pharmaceutical interventions. If you are a clinical director or neuro-ophthalmologist, it’s a cue to engage with emerging standards for trial design, endpoint measurement, and cross-disciplinary collaborations between neuroscience and engineering.
If you are a policy leader, it’s a prompt to assess how regulatory frameworks can balance innovation with patient safety without stifling either.
The potential to restore vision – even in cases once deemed irretrievably blind – is a profound leap. However, the distance between potential and practice remains measurable in rigorous human evidence, safety validation, and economic models that justify adoption at scale.
FAQs
1. What does the FDA Breakthrough Device designation actually mean for Neuralink’s Blindsight?
It means the FDA will provide faster, more frequent regulatory engagement for Blindsight, not that the device is proven effective or approved for market use. The designation accelerates review processes, but clinical evidence thresholds remain unchanged.
2. Is Blindsight close to being available for patients with blindness?
No. Blindsight is still in early clinical development. Human trials will focus first on safety and basic signal interpretation, not full functional vision restoration. Commercial availability remains years away and contingent on trial outcomes.
3. How is Blindsight different from existing treatments for irreversible blindness?
Blindsight bypasses the eye and optic nerve entirely by stimulating the visual cortex directly. Existing approaches, such as gene therapy or retinal implants, depend on partially functional retinal or optic pathways, which limit their applicability.
4. What evidence exists today that Neuralink’s brain implants work in humans?
Current peer-reviewed human evidence supports neural signal decoding for digital control tasks in individuals with paralysis. There is no published human data yet demonstrating restored or meaningful visual perception.
5. Why does Blindsight matter to health-system leaders and biotech investors now?
The FDA designation signals regulatory openness to invasive neuroprosthetics for severe unmet needs. That shifts investment and research conversations from speculative neuroscience toward regulated clinical infrastructure, reimbursement strategy, and long-term safety evaluation.
Dive deeper into the future of healthcare. Keep reading on Health Technology Insights.
To participate in our interviews, please write to our HealthTech Media Room at info@intentamplify.com