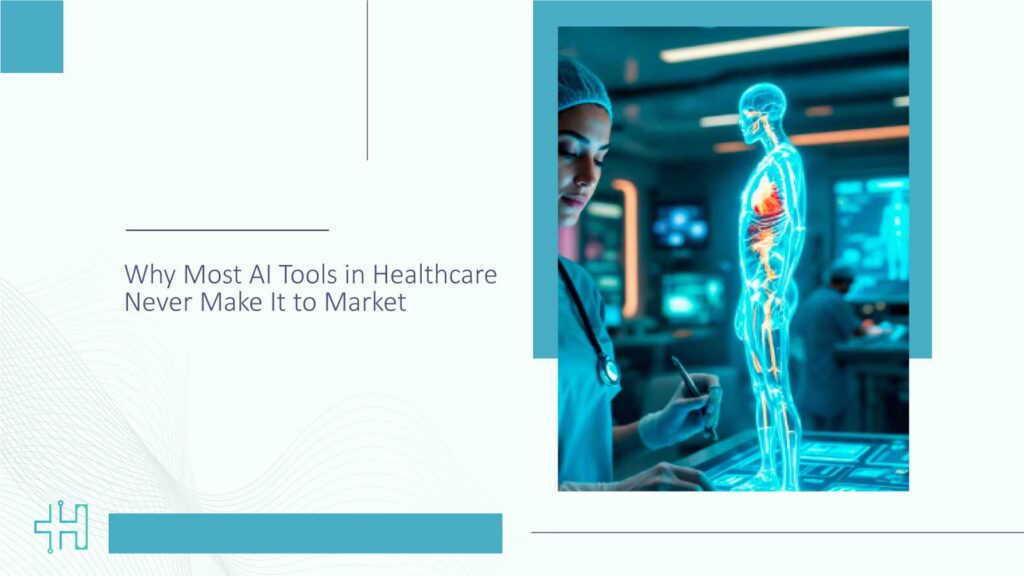
Every few weeks, we hear it: a new AI breakthrough that’s going to “revolutionize healthcare.” It might predict cancer from a blood test. Or generate clinical notes with near-human precision. Or help overloaded physicians triage patients more effectively. The promise sounds irresistible. Yet for all that hype, most AI tools in healthcare never make it to real-world use.
This is not because they fail in the lab. But crossing that last mile, from research prototype to bedside tool, is far harder than it looks.
This article explores why that happens. Why tools with promising models, strong data, and even published validation studies often get stuck in what insiders call the “AI valley of death.” More importantly, what leaders across health systems, startups, and regulatory bodies need to rethink if we want AI in healthcare to deliver on its promise.
Great Accuracy Doesn’t Mean Great Usability
Let’s start with something that surprises people outside the industry: clinical accuracy is not the main reason AI tools get rejected.
Sure, performance matters. But a model that predicts patient deterioration with 91% accuracy doesn’t help much if it can’t explain why, or if it interrupts a nurse’s workflow at 2 a.m.
In healthcare, usability isn’t a bonus feature. It’s the core requirement. Clinical environments are chaotic. Nurses and physicians juggle dozens of inputs per hour. They don’t have the time (or mental bandwidth) to decipher a black-box recommendation or learn a new app in the middle of a shift.
Real-world clinicians need AI that fits in, not stands out.
That’s why the most successful tools don’t just focus on precision. They integrate with the EHR. They align with existing alert systems. They’re quietly helpful, not obtrusively brilliant.
Take Mayo Clinic’s AWARE system, for example. It doesn’t wow anyone with flashy algorithms. But it’s deeply embedded in clinical workflows, and that’s exactly why it works. Studies have shown it reduces ICU cognitive load and improves decision-making without overwhelming staff.
Now imagine how many startups skip this step, focusing on model performance in isolation. It’s like designing a racecar engine and forgetting the steering wheel.
Validation Doesn’t Equal Trust
It’s tempting to think peer-reviewed studies or FDA clearances should be enough to get AI tools deployed in hospitals. And to be fair, that used to be true, sort of.
But healthcare decision-makers today are more cautious. They’ve seen AI tools rolled out too early, without real-world guardrails, only to be pulled back months later. Some were biased. Some failed in edge cases. Some just didn’t work well in their specific populations.
Validation in one setting doesn’t guarantee performance everywhere.
A Nature study reviewed over 170 published AI tools in healthcare. Only a small fraction had any external validation. And even fewer showed consistent accuracy outside their training environment. It’s a wake-up call: algorithms are not universal. Healthcare is messy, and local context matters.
But trust goes deeper than data.
Hospital leaders want to know: What happens when this model makes a mistake? Who’s accountable? Will it learn from local outcomes? Can I explain this to my board, my legal team, and my front-line clinicians?
Until those questions are answered, clearly and credibly, even “validated” tools will sit on the shelf.
Interoperability Is the Elephant in the Room
We don’t talk enough about this. But even the most brilliant AI tool can’t do much if it can’t plug into the existing health IT ecosystem.
And that ecosystem? It’s a tangle of legacy systems, siloed data, and slow-moving procurement processes.
EHRs weren’t built with AI in mind. Many health systems still struggle to get basic data out of them in real time. Now imagine trying to integrate a machine learning model that needs clean, continuous inputs from multiple systems, lab results, imaging, notes, and vitals, all in sync.
It’s no surprise that so many promising pilots fizzle out in deployment.
The most agile AI tools in healthcare today aren’t the smartest. They’re the most integrable. They’re built with FHIR compatibility, API-based workflows, and modular architectures from day one. They assume delays, missing data, and partial integrations, and still manage to deliver value.
But that kind of thinking is rare.
Too many AI developers underestimate the complexity of healthcare IT environments. They build for the ideal world, not the real one. And as any CIO will tell you, the real world is where good ideas often go to die.
The Translation Gap in Healthcare AI
If you’ve ever marveled at an AI demo during a healthcare conference and thought, “Why isn’t this in every hospital yet?” you’re not alone. Many groundbreaking AI tools in healthcare dazzle in research papers, impress onstage, and generate media buzz. But the journey from publication to practical use? That’s where most of them quietly stall.
Let’s unpack why that happens and why it matters more than ever.
A Solution in Search of a Workflow
Here’s a truth that rarely makes it into the headlines: brilliant AI often fails not because it’s bad, but because it wasn’t built with frontline reality in mind.
Take clinical workflows, they’re not just a checklist of tasks. They’re a complex web of timing, trust, and triage. When an AI tool requires clinicians to stop what they’re doing, open another interface, or learn a new protocol mid-shift, it disrupts more than it supports.
Now imagine pitching that to a burned-out physician juggling patients, EHR alerts, and administrative overhead. Unless the AI slides in seamlessly, think smart suggestions inside the tools they already use, it’s unlikely to survive.
The Lab Isn’t the Hospital
Academic validation is important. It gives AI tools a chance to prove themselves. But models trained on retrospective data, under ideal conditions, don’t always translate to the chaos of live care settings.
Let’s put this into perspective: a study in npj Digital Medicine found that 72% of published healthcare AI models failed when tested outside the environment in which they were trained. Source
Why? Because real-world patients don’t follow the rules. Their symptoms overlap. Their data is messy. And hospitals vary dramatically in their workflows, software, and even patient demographics.
In other words, an algorithm that excels in Boston may sputter in Baton Rouge, not because it’s flawed, but because healthcare isn’t one-size-fits-all.
Evidence Isn’t Enough, You Need Buy-In
One of the most overlooked hurdles is human adoption. Clinicians want to trust their tools. They want transparency. And they want assurance that using AI won’t open them up to legal or ethical blowback.
So, even if your AI shows a 95% accuracy rate in flagging sepsis, if it’s a black box, or if it slows down decision-making, chances are it will be met with hesitation or outright rejection.
This is where many developers misstep. They approach AI as a product, not a partnership. But in healthcare, adoption is emotional as much as it is technical.
Why This Matters Now
As generative AI evolves, we’re seeing more tools aiming for bedside impact, from ambient clinical documentation to diagnostic support. The stakes are getting higher. So are the expectations.
But unless developers start co-creating with clinicians, not just testing on them, most AI tools in healthcare will continue to live in limbo: peer-reviewed, demo-ready, but rarely deployed.
What This Means for Innovators and Investors
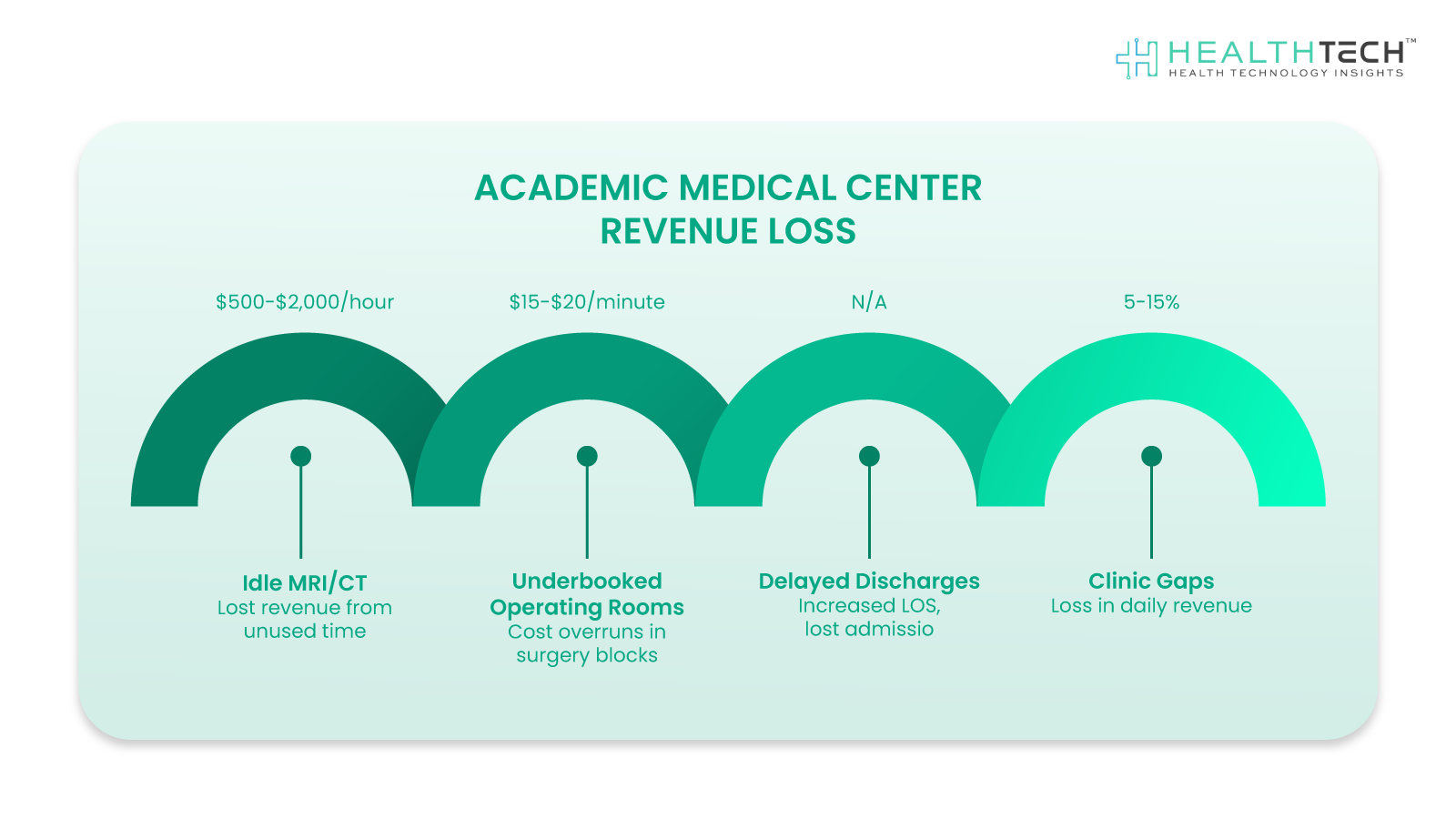
Everyone in healthcare talks about “value,” but few define it the same way.
- For startups, value often means innovation speed and funding runway.
- For clinicians, it’s saved time and safer care.
- For hospital leaders, it’s outcomes, yes, but also workflows, budgets, and risk.
And for investors? It’s that golden trio: scale, stickiness, and proof that someone’s willing to pay for it again.
The hard part? All of these must align in one of the most complex, regulated industries on Earth.
So, Where Should You Focus?
Whether you’re an AI founder building your next tool or an investor scanning the post-LLM healthcare landscape, here are three hard-won lessons that keep coming up:
1. Solve a “Tuesday Morning” Problem
If your solution isn’t useful on a random Tuesday morning, when the ER is slammed, the EHR is lagging, and nurses are short-staffed, it won’t get used.
In other words: don’t aim for flash. Aim for quiet utility.
The best AI tools in healthcare don’t shout. They slide in. They remove friction. They make a tired clinician’s job feel slightly more doable.
2. Don’t Just Show Accuracy, Show Adoption
A 92% model accuracy means little if the interface slows down patient rounds or generates more follow-ups than it solves.
What clinicians (and health systems) want to know is:
- How fast is it?
- Does it work in their workflow, not just a pilot site’s?
- Will it play nicely with the tools they already use?
Case studies with real adoption data, not just “we could,” but “we did”, carry more weight than any academic benchmark.
3. Invest in Trust, Not Just Tech
Here’s what’s often overlooked: your brand reputation will be shaped less by your algorithm and more by how you handle edge cases, downtime, or pushback.
- Are you transparent about what your model can’t do yet?
- Are you investing in explainability, not just outcomes?
- Are you building feedback loops with clinical teams, or around them?
Trust isn’t a switch. It’s a slow build. But in healthcare, it’s the difference between a one-time deployment and long-term loyalty.
Final Thought: The Next Healthcare Unicorn Will Be Brilliant
Not boring as in uninspired, but boring as in sustainable.
- It will solve real operational headaches.
- It will empower frontline staff without disrupting them.
- It will be vetted, validated, and woven into the fabric of care, not tacked on top.
So if you’re dreaming big in AI and healthcare, don’t just chase shiny.
Chase meaningful. Chase usable. Chase trusted.
That’s where the real transformation and returns live.
FAQs
1. Isn’t ChatGPT already doing a lot? Why do we need RAG at all?
Although ChatGPT excels at a conversation or overview of general information, RAG does it a step better by introducing real-time, reliable sources such as patient records, medical studies, or hospital policy into the equation.
2. Can we ever rely on AI, such as RAG, with something as personal as healthcare?
Completely reasonable to be wary. RAG isn’t designed to cut out doctors or nurses; it’s designed to assist them, particularly when there’s more data and less time.
3. Where would I observe RAG in action within a hospital?
Good question. You’ll most likely see RAG quietly behind the scenes, enabling things like auto-filling clinical notes, assisting with triaging incoming cases, or distilling huge stacks of medical research into actionable insights.
4. What makes RAG safer or more reliable than legacy AI tools?
Here’s the big difference: RAG demonstrates its work. Rather than guessing or imagining answers, it takes information from verifiable sources. That way, clinicians can know where a suggestion originated.
5. Do hospitals need an entirely new technology setup to implement RAG?
Not at all. One of the beauties of RAG is that it’s something you can easily integrate into tools and workflows you already have, whether that’s your EHR platform or a clinical decision support tool.
Dive deeper into the future of healthcare.
Keep reading on Health Technology Insights.
To participate in our interviews, please write to our HealthTech Media Room at sudipto@intentamplify.com